ACL Reconstruction
What is an ACL reconstruction?
An anterior cruciate ligament (ACL) tear or rupture can lead to symptoms of knee instability. If untreated, these episodes of instability can potentially result in secondary damage to the menisci in the knee and cause accelerated arthritis. If you sustain an ACL injury, an ACL reconstruction can be performed to restore the stability of the knee. An ACL reconstruction involves harvesting a graft to replace the torn anterior cruciate ligament, restoring the knee's stability.
Mr Pai is experienced in performing ACL reconstruction in children. You can read about the differences compared to adult ACL surgery here.
What is involved in an ACL reconstruction?
The steps involved in anterior cruciate ligament reconstruction surgery include:
1. Knee arthroscopy
Key-hole surgery is performed to confirm the ACL tear and identify secondary injury to the cartilage and meniscus. Any secondary injuries are treated during the same procedure.
2. Graft harvest
A donor graft is harvested, prepared, and used in order to replace the torn ACL. This can be the hamstring tendons, patellar tendon, or quadriceps tendon. The choice of graft is discussed between you and Mr Pai during your consultation and depends upon your sporting and work demands. For a majority of patients, a hamstring or quadriceps graft is a suitable choice.
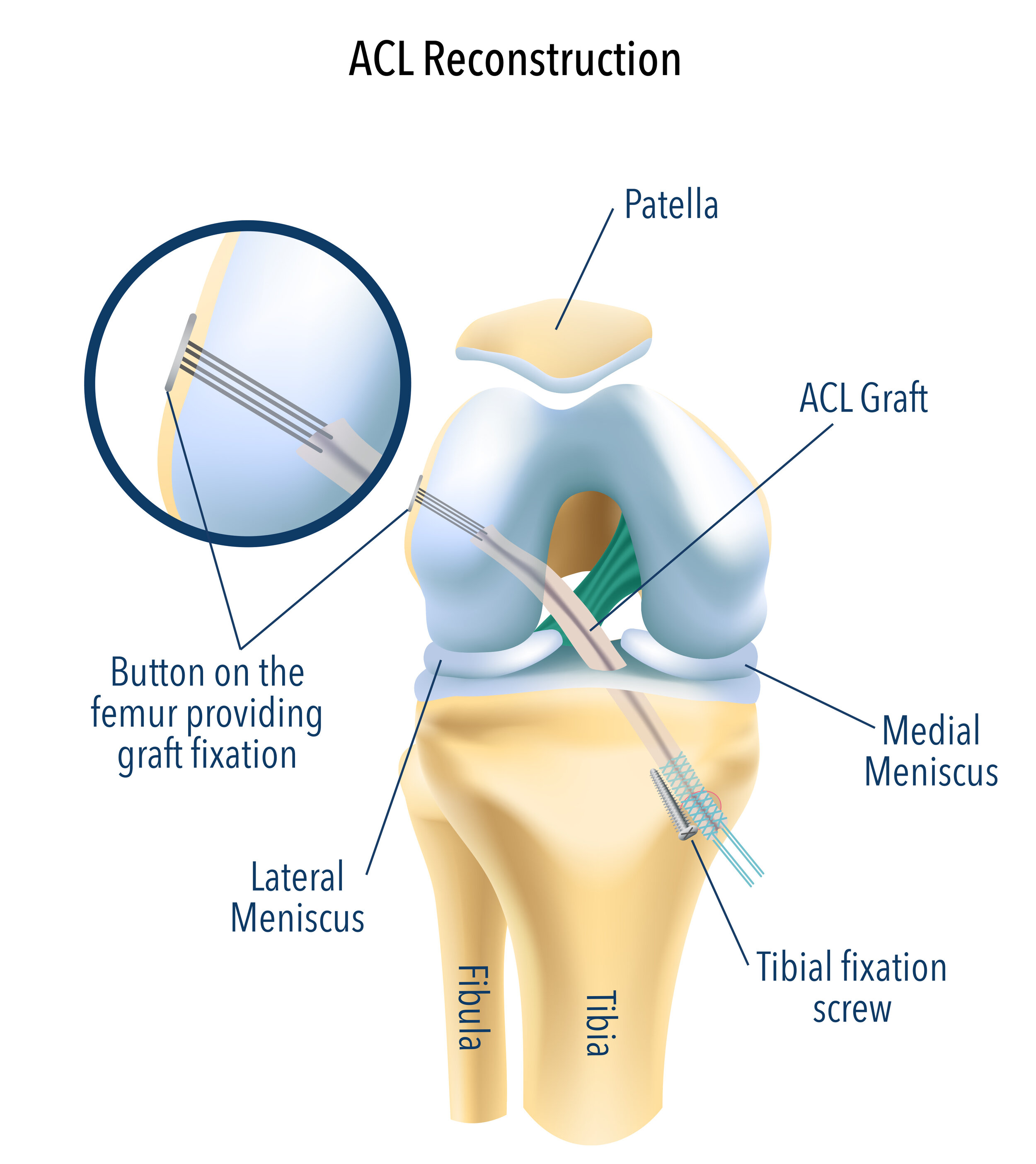
3. Tunnel drilling
Bone tunnels are created within the femur and tibia in a location that simulates ACL origin and insertion. The tunnels are required to allow passage of the graft. An accurate bone tunnel is important so favourable forces can pass through the ACL graft. An improper tunnel position can cause early re-rupture of the graft and is a common technical cause of graft failure.
4. Graft passage and fixation
The graft is passed through the bone tunnels and fixed into place with screws or over a loop of strong sutures threaded to a button.
5. Lateral extra-articular procedure (LEAP)
A LEAP is performed in patients at high risk of re-injuring their ACL graft. This group includes young athletes, individuals undergoing revision ACL surgery, patients with knee hyperextension, and those exhibiting significant rotational instability during knee examination. The procedure involves harvesting a strip of tissue from the iliotibial band on the outside of the knee. This tissue is then re-routed beneath the lateral collateral ligament and securely re-attached. The primary aim of the LEAP procedure is to enhance rotational control of the knee and reduce instability following ACL reconstruction. Read more about a LEAP and its benefits.
What is my follow-up schedule after the operation?
Approximately 3-4 weeks of leave from work is required for a desk-based job.
2 weeks
The wound dressings will be removed, and the wound will be reviewed to ensure it has healed. At this stage, the sutures will also be removed.
8 weeks
The range of motion in the knee will be assessed. You should be able to fully straighten the knee and bend it more than ninety degrees.
4 months
The range of motion and strength of the knee will be assessed. By this stage, you should have a near-normal range of motion. A small amount of residual swelling within the knee can be expected at this time point.
12 months
After completing a supervised post-operative course of rehabilitation, a referral is made for return-to-play testing to ensure you are safe to return to sport.
Frequently Asked Questions
What are the risks of having ACL surgery? +
General complications of ACL reconstruction surgery can include:
Infection
The risk is less than 1 in 400 of developing an infection. This can occur despite using a sterile surgical technique, giving pre-operative intravenous antibiotics, and soaking the graft tissue in antibiotics.
If the infection involves only the wound (superficial), it may just need treatment with a course of antibiotics.
If a deep knee joint infection occurs, it may require more surgery to wash out the knee as well as intravenous antibiotics. If the infection fails to resolve after this, the graft tissue may require removal.
Deep vein thrombosis and pulmonary embolism
Clots can occur in the deep veins of the leg that may dislodge and occlude the arteries in the lungs. DVT presents as leg pain and swelling after your operation. The diagnosis is confirmed with an ultrasound scan and, depending on the type of DVT, may require treatment with blood thinners.
Bleeding and haematoma formation
Small vessels at the surgical site continue to bleed post-operatively and cause swelling, bruising, and pain. Although most cases resolve with time, some will require a washout of the pooled blood beneath the surgical wounds.
Specific complications of ACL reconstruction surgery can include:
Saphenous nerve damage
This can occur when the hamstrings are harvested and will result in a numb patch on the inside of the leg. This usually improves with time but occasionally can be permanent. This does not affect the function of the ACL graft.
Difficulty kneeling
Patella tendon harvest is performed with an incision directly over the tendon at the front of the knee. As a result of the incision and the location of the graft, kneeling on the operated knee is sometimes poorly tolerated.
Patella fracture
Harvest of the patella tendon with the associated patella bone can weaken the integrity of the patella. This may result in a fracture of the patella. This usually requires surgical correction if it occurs.
Graft re-rupture
Despite adequate rehabilitation, an ACL graft may fail. The risk is highest in the first year following ACL reconstruction, but is still higher than baseline between 1-2 years post-operatively. The risk is higher in younger patients. If this occurs, Mr Pai will talk to you about the option of revision surgery.
Stiffness
The knee can become stiff after surgery due to the formation of scar tissue. This stiffness usually resolves with physiotherapy but can sometimes persist. If the knee is not bending or straightening adequately 6-8 weeks post-operatively, a manipulation procedure may be required. This involves putting the patient to sleep and pushing on the knee in order to break the scar tissue.
Long-term osteoarthritis
Despite having an ACL reconstruction, the risk of developing osteoarthritis in the long term is higher than for the general population. This is because the cartilage damage that occurs at the time of injury is irreversible.
Why do ACL tears happen? +
ACL tears occur because the knee is placed in a disadvantaged position and is unable to withstand the rotatory force being put through it. This can be due to muscle fatigue or poor biomechanics. To get an ACL tear, the knee has to partially dislocate. Some patients are more susceptible to ACL tears due to variations in their anatomy which put more stress on the ACL.
Can I reinjure my reconstructed ACL? +
Although the tissue used to reconstruct your ACL is biomechanically stronger than your native ACL, there is still a risk of reinjury to your reconstructed ACL. It is important to follow the post-operative instructions provided by Mr Pai and your physiotherapist to minimise that risk. The risk is highest in the 12 months following your reconstruction, but is also slightly higher in the 12-24 month period. Prior to returning to sport, it is important to ensure that your muscle bulk is symmetrical to the uninjured side and that you have good control of your knee with the ability to perform single leg squats, hops, and other plyometric exercises. We will refer you to a physiotherapist for return to play testing within a suitable timeframe post-operatively.
Am I at risk of having an ACL injury on the other side? +
As patients who have ACL injuries generally have intrinsic factors that predispose them to ACL rupture, they are at a higher risk of having an ACL injury on the other side.
How can I prevent this injury from happening? +
Prior to playing sport, certain exercises have been shown to decrease the risk of ACL injury if they are performed regularly. It is best to incorporate these exercises as part of your warmup regime.
The main components of these exercises include:
- Core training - Hip and trunk muscles
- Neuromuscular control and balance - Jump and land techniques
- Plyometrics and agility
- Strength training of the Quadriceps & Hamstrings
Do I need an ACL reconstruction for my ACL tear? +
This depends on your level of activity and expectations. In low-demand patients that are not involved in sport that involves rapid changes in direction, it is appropriate to trial a 4-month period of physiotherapy to strengthen the muscles surrounding the knee. Conditioning these muscles may provide enough stability so a low-demand patient can continue their activities.
In a younger athlete actively involved in sport, an ACL reconstruction is recommended to restore the stability within the joint. The argument for surgery is strengthened if there is a concurrent repairable meniscal tear as this can be repaired at the same time as the ACL reconstruction. The stability provided by an ACL reconstruction can prevent further damage to the meniscus.
Patients with an ACL tear and a repairable meniscal tear that continue to play sport without a reconstructive operation are likely to sustain further meniscal damage and will inevitably develop knee arthritis early.
If an ACL tear is being managed non-operatively, it is important to work with a physiotherapist and rehabilitate the knee. This will help strengthen the muscles surrounding the knee and improve your balance. Reassess your symptoms after a 4-6 month period of rehabilitation and reconsider surgery if your knee still feels unstable.
Without an ACL reconstruction you should be able to run, cycle, swim, play doubles tennis and possibly ski. As long as you trust your knee and it feels stable during activity, you can push the boundaries.
Am I too old to have an ACL reconstruction? +
There is no fixed age limit when you can have an ACL reconstruction. The decision to proceed with surgery is multifactorial and will depend on the presenting symptoms, the duration of time you have had an ACL tear for and the presence of cartilage damage or arthritis within the knee. If you are uncertain about whether an ACL reconstruction is in your best interests, Mr Pai would be happy to provide a balanced opinion about the management of your knee.
What is a lateral tenodesis and how does is help reduce ACL graft reinjury? +
A lateral tenodesis involves taking a strip of tissue (1cm thick and 8–10cm long) from the iliotibial band on the outer side of the knee and re-routing it beneath the lateral collateral ligament. It provides additional rotational control of the knee. It is performed at the same time as an ACL reconstruction in selected patients as it reduces the risk of an ACL reinjury.
Read more about lateral tenodesis.
I have a torn meniscus as well as an ACL injury, will you repair the meniscus at the same time? +
Preserving and repairing the meniscus is always preferable to removing it. The meniscus acts like a cushion to support your cartilage. Having a torn meniscus is a common associated injury when you have an ACL tear. Any meniscal tears will be treated at the same time as your ACL reconstruction. If a meniscal repair is performed, it will slow your rehabilitation for the first few weeks as the repair needs to be protected. However, thereafter you will resume your ACL rehabilitation as normal. The advantage of performing the meniscal repair at the same time as the ACL reconstruction is that the repair is more likely to be succesful. The bleeding into the knee that occurs after an ACL reconstruction is rich in growth factors which promotes tissue healing.
Read more about meniscal repair.
When can I walk after an ACL reconstruction? +
You will be walking and bearing weight with crutches on the day of surgery after an ACL reconstruction. Crutches are used to make walking and bearing weight comfortable. Most patients require them for 1-2 weeks after surgery. A post-operative brace is not required unless a meniscal repair was performed at the same time. If a concurrent meniscal repair was performed you may require a brace and up to a 6-week period of not bearing weight on the operated side.
When can I drive after an ACL reconstruction +
You will not be able to drive for 6 weeks following an ACL reconstruction. You must be off strong painkillers, be walking without crutches and have a relatively painfree range of motion in the affected knee before your commence driving.
When can I swim after an ACL reconstruction? +
The wound should be kept dry for two weeks following the operation. Once the wound healing is reviewed at your 2-week post-operative consultation you will be able to shower with no wound dressings on. Participating in pool based rehabilitation or swimming is not recommended for 4 weeks after your operation as it may increase the risk of infection.
When can I return to playing sport after ACL surgery? +
There are various factors that determine when someone can return to playing competitive sport after having an ACL reconstruction. It is crucial to make sure that the ACL graft has healed adequately and that the athletes muscle strength and control has returned to near-normal levels before returning to sport. This usually occurs at a minimum of 12 months after the operation.